
Conclusion:Early outcomes after surgery for IAA/VSD in neonates and infants are satisfactory. The patient who received Yasui operation experienced no residual obstruction during the follow-up. A total of 17 patients received 21 reoperations. Freedom from left ventricular outflow tract (LVOT) obstruction at 6 months, 1 year, 5 years after surgery was 91%, 83% and 73% respectively. Freedom from aortic arch obstruction at 6 months, 1 year, 5 years after surgery was 75%, 72% and 72% respectively. Median follow-up time was 3.5 years (range, 1-10 years). Duration of cardiopulmonary bypass longer than 135 min, surgery received during neonatal period and before 2016 was identified as higher risk group for mortality. Results:Early mortality after surgery was 13%. Risk factors for early mortality was analyzed by decision tree model. One-hundred-and-twenty-two patients (99%) underwent standard aortic arch reconstruction with VSD closure, and one neonate (1%) underwent staged Yasui operation. Methods:This was a retrospective review of clinical data of 123 neonates and infants who received surgery for IAA/VSD from Jan 2009 to Jan 2019. Whichever way they are categorized, it is helpful to have a working understanding of normal and fetal circulation, as well as an understanding of the segmental approach to imaging in congenital heart disease.ABSTRACT Objective:To summarize the surgical outcomes of interrupted aortic arch with ventricular septal defect (IAA/VSD) in neonates and infants. There is more than one way to present the variety of congenital heart diseases. short segment severe aortic coarctation.General differential considerations include: Surgical correction (either single- or multistage) is the definitive treatment. Prostaglandin E 1 may be given to initial management to keep the ductus open. If uncorrected, it carries a very poor prognosis with extrauterine survival being as little as a few days. great vessels may show a "V" configuration on coronal imaging 2.non-visualization of the portion of interruption.CTĪllows visualization of the interrupted aortic arch and associated anomalies. These modalities may not allow differentiation of IAA from severe aortic coarctation with a hypoplastic arch 9. The ascending aorta may also appear more vertical than usual. The right ventricle may appear a lot larger than the left, although this is a non-specific finding.
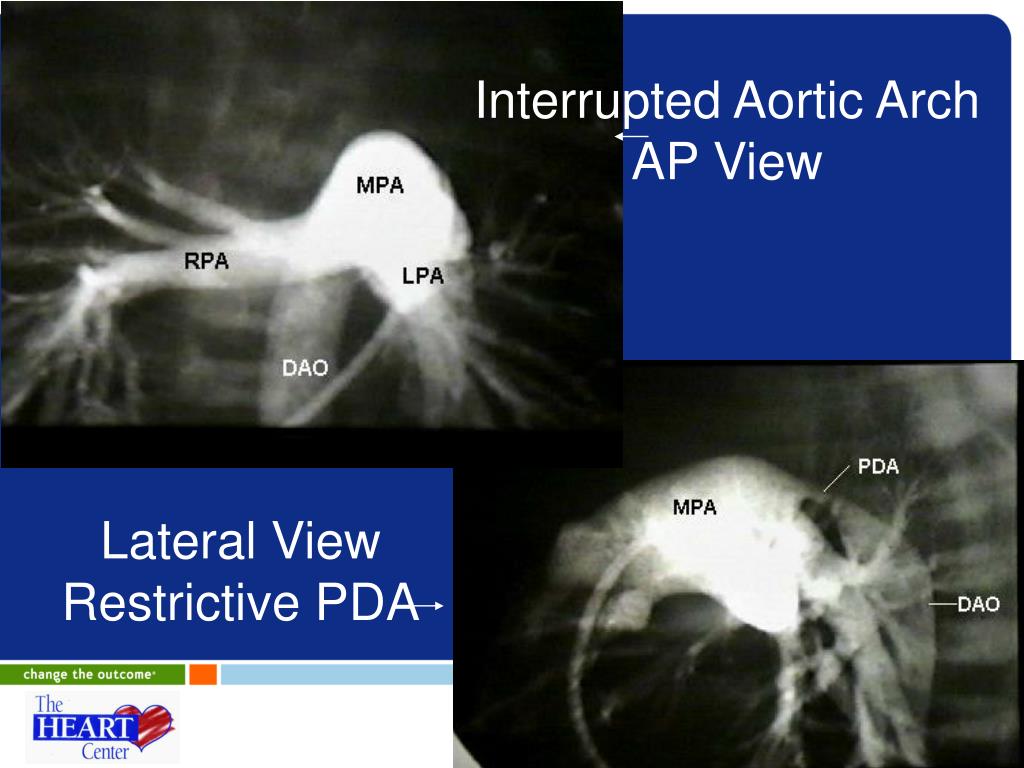
Plain film features are often non-specific 3: aortopulmonary septal defect (aortopulmonary window).almost always associated if there is a right-sided descending aorta.found commonly in those with a type B interruption.subtype 3: isolated subclavian artery that arises from the ductus arteriosus.type C: rare, interruption occurs proximal to the left common carotid arterial originĮach type is divided into three subtypes 7:.type B: most common (>50%), the break occurs between the left common carotid and left subclavian arterial origins.type A: second most common, the interruption occurs distal to the left subclavian arterial origin.ClassificationĪccording to the Celoria-Patton classification, IAA can be classified into three types according to the location of the anomaly: Pathologyįaulty embryological development of the aortic arch (thought to occur during the 5 th to 7 th week of intrauterine life). It may account for ~1.5% of congenital cardiac anomalies.


 0 kommentar(er)
0 kommentar(er)
